The next couple weeks were focused on recovery and rest. My family took excellent care of me. I’m very careful with my diet – eating only soft foods, soups and lots of smoothies. Friends and family inundate me with flowers and get well cards and I catch up on a lot of movies.
I saw my surgeon in his office. He hinted at cancer but never made a direct statement. The biopsy was supposed to take 5 days, but this tumor isn’t common, so it had been shuffled to different labs for verification before final results were sent back to him. He is pleased with how the incision is healing and approves longer walks and light jogging.
When the surgeon finally calls with the results more than 14 days post-surgery, he tells me it’s a gastro-intestinal stromal tumor (GIST) and lets me know surgery was probably the only treatment needed. I take that to mean it was not cancer. He asks me to see an oncologist to confirm treatment.
I got a recommendation for a gastro-oncologist and head over thinking this is going to be a short and semi-pointless consult. I’m retelling my story, he’s reviewing the reports, and then he looks at me and says, ‘So it looks like your in remission…’ I immediately interrupt and say, ‘Wait, what? Remission? That’s a term you use when talking about cancer’. He can see plain as day I haven’t heard any direct statements, so he pauses and then he patiently restarts from the beginning.
He states that the tumor is cancer.
He defines the type (sarcoma) and explains various details, he answers all my questions until I’m just sitting in quiet disbelief. It’s not a short appointment. My husband is with me and is just as rattled as I feel. We head home and the anxiety floods in. What does this mean?
I dive into researching every last word on every report – the surgical report, the ct reports, the biopsy results. I get genetic testing done, I have a coloscopy & endoscopy, there are more biopsies sent out. I get second and third opinions. I talk to my family and friends. My sister works in a hospital setting and we discuss every last detail of every appointment, every opinion, and every report. She uses her access to scientific research to precure more information. I have more appointments with the oncologist.
Every time I felt like I reached a level of understanding or felt a sense of security with the situation, the next doctor appointment or scan result would rip that footing away and I’d be spinning in a sea of anxiety.
The worst one was a follow up CT scan they did to inspect my other organs for evidence of cancer. I had been told over and over again that there was no evidence that the cancer had metastasized – ie – it had not spread past the one tumor. This scan was simply part of the standard treatment routine. My tumor was medium risk based on how fast it had been growing, and it was stage 2. Stage 2 is good – that’s early – and you know what everyone says, when you catch it early, better outcomes.
The doctor called and told me they found a spot on my liver.
The liver and the lungs are the 2 organs that this type of cancer metastasizes to first. I’d learned that from the doctors and from the internet research I’d done. Now, he also said there’s not need to panic, it could be any number of things, but I’d need an MRI to better view it and determine if it’s part of the cancer.
For the majority of this experience, and up until this point, I had been able to keep a level of hopefulness and positivity going. This news, however, broke me. Suddenly, not seeing my kids graduate high school was a real possibility. I’d miss their birthdays, their milestones. I’d miss seeing them create their own families. Should I pre-write birthday cards for them, and how many? Would getting a birthday card from me after I’m dead make them feel loved or just create unnecessary heartache? The unfairness and randomness of it all was crushing and I absolutely lost it.
The good part of COVID is that with everyone hunkering down at home, I’m able to schedule appointments very quickly. I get the follow up MRI done a couple days later and the doctor calls with results that same day letting me know that the spot on my liver is not part of the cancer.
I’m elated… for the moment.
The roller-coaster of emotions wasn’t limited to just doctor calls, there’s the experience of telling my friends and family it’s cancer. As if this whole situation isn’t stressful enough, waiting for and dealing with their reaction is rough – everyone is initially shocked, which makes sense, but then many seem afraid – afraid of the word, afraid for me or afraid of me – sometimes all three. It’s surreal.
With most people though, we are able to get past that initial awkwardness and get to a real discussion. Talking about it helps me process what’s happening, it helps me solidify my understanding, so I talk a lot.
I’ve never experienced this level of emotional turmoil – the ups & downs were drastic in the first couple months post surgery and I’d have days where I just had to shut off – I couldn’t focus on work for any length of time or accomplish simple household chores. It was just sit in the backyard, toss a ball for my dog or sleep.
I am so grateful to have such incredible people – family & friends – in my life helping me get through all of this. My husband Jason, my sister Debbie – I would have been a disaster without them.
I’m a year out now, and am back to life-as-normal, but there is an undertone of anxiety that lingers. Once in a while it’ll rear back up – a doctors appointment or periodic scan for example. It’s always there, nagging quietly in the back of my mind. I’ve spoken to a lot of cancer survivors who have a similar experience – the anxiety never leaves, but it does fade into the background.
I try and use it as a reminder to appreciate what I have right now and to take action on my bucket list items rather than wait. And if I need a day to tune out, I take it.
Meanwhile, I’m frustrated by how long soft tissue takes to heal.
Some days were good, some days were not. I had to be careful with what I ate, and once in a while my intestines would act up. At one point, about a month after a my surgery, I got that “backed up” stomach ache that started this whole fiasco – it felt like another intestinal blockage.
Off to the urgent care I went for yet another CT scan. They found that my intestines’ were indeed blocked again. The intestines appeared ‘flattened and closed’ at the surgery spot. They could see swelling before the surgery point and deflation after that point – like a balloon pinched closed between your fingers. Sometimes the scar tissue can stick to itself they told me, causing this type of blockage.
They transferred me to the hospital. I did not want to be here. I did not want to go through this again.
My surgeon looked at the films and had everyone wait. Sometimes, he said, if the scar tissue isn’t healed together, this type of blockage can sort itself out with hydration and laxatives. The pain had receded so that was a good sign. They pumped me full of fluids and after a few more hours passed the surgeon stopped by to poke and prod my abdomen. He determined that the blockage had indeed cleared on it’s own and I sent home without any other treatments.
As the days and weeks pass without any other complications, my desire to become more active, specifically to ride my bike, kicked in.

When can I start riding again?
I walked everyday – after most meals, especially if I had any odd stomach aches or pains. I worked up from struggling to get around my neighborhood block without stopping to a few steady miles. My dog is super energetic and strong, so I spent the early weeks diligently training him to not pull or chase squirrels on our walks. The surgeon was very clear that I had to be careful not to lift or strain while my abdomen healed. There was a lot of freshly boiled chicken involved. We slowly progressed to jogging and I rekindled an long-passed passion for running. After what felt like an eternity I was able to return to riding.
I was happy to be on two wheels, but my body was not right and the idea of training or racing seemed very distant. Despite this, I stayed positive, and approached recovery like any other goal:
- clarify the big-picture,
- figure out the steps to get there,
- focus on 1 step at a time,
- celebrate small achievements &
- accept that this would be a lengthy journey.
I’d ride a few miles feeling great and then my back wheel would slip on gravel or wet rocks and it would feel like I sprained my abs. I avoided riding in any wet conditions whatsoever, and had to avoid technical trails and features (my favorite stuff). I bridged this weakness by getting my dog Odin a sled harness and bungee leash so he could do the pulling when conditions were less than ideal. I also started a home physical therapy routine targeting my abs and cupping for the scar tissue.
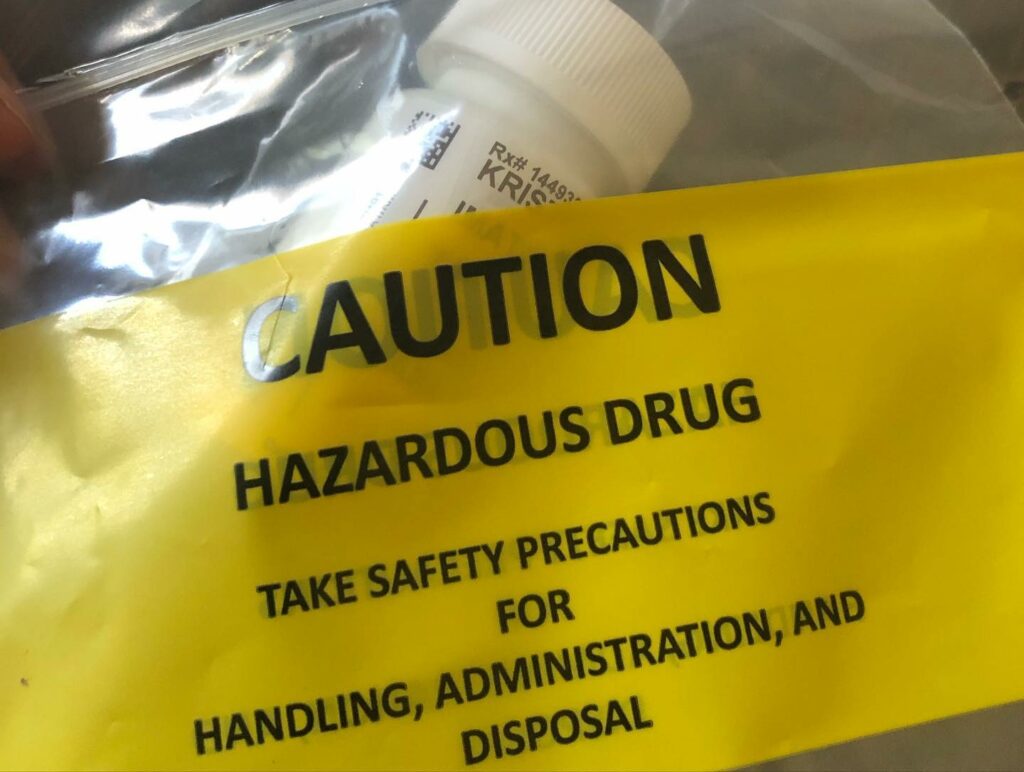
Part of my cancer treatment is taking imatinib (gleevec) for at least 3 years.
It’s a chemotherapy drug that has minimal side-effects relative to what you’d normally think of when someone say’s “chemo”. The side effects were stronger initially – nausea, upset stomach, fatigue, flu-like symptoms & muscle cramps – but I’ve adjusted to the medicine and can deal with the lingering issues that pop up – I go to bed earlier or take an afternoon nap, I take magnesium and electrolytes for the muscle cramps and I have an anti-nausea med to combat any upset stomach.
Returning to Glen Park
In the back of my mind this whole time I’m weighing whether or not returning to racing is a reasonable expectation. I find true happiness on my mountain bike – that feeling of flying through the woods – I love it. I also find great joy in the process of setting, pursing and achieving goals – racing gave me a clear set of targets, but I don’t necessarily need to race to find contentment, so I decide that I’d be okay with not racing anymore if my body just can’t take it.
As the fall of 2020 rolls in, an enduro at Glen Park opens registration. I love Glen Park! But I am pretty far from anything that looks like ‘race shape’. What the hell – it’s a day on my bike at a place I love seeing people I like – that’s more than enough to convince me to sign up.
My teammates & I head to the park the weekend before the race to get some extra time in on the trails. That double that scares the crap out of me? What do I have to lose by going for it? Today, I’m feeling good, tomorrow, I might not. Let’s not wait another day. I clear it.
I have to do it again. And again. [You can watch it here: https://www.facebook.com/1487105181551108/videos/1904567559673805 ]
The following weekend the race is hard, but it’s an epic day. I’m exhausted by the back to back riding – pre-ride & race day. Between the meds & my poor fitness, recovery is harder than ever, the muscles cramps are vicious at night after a hard day workout, but I’m so happy to be out there, that none of that matters.
By the end of the day I find myself standing on the top step of the podium and I’m pretty emotional. I can see a path back to racing – this chapter doesn’t have to close just yet – which is good because I’ve got a few bucket list items to knock off my list first.